What is Pulmonary Embolism?
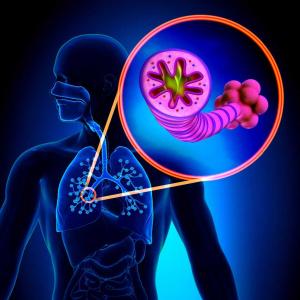
Pulmonary embolism, medically known as pulmonary embolus, is a life-threatening condition that occurs when a pulmonary artery, which supplies blood to the lungs, becomes blocked by a blood clot (thrombosis). The clot usually forms in the deep veins of the legs (deep vein thrombosis) and travels through the bloodstream to the lungs. Therefore, deep vein thrombosis (DVT) is often the underlying cause of most pulmonary embolism cases.
The blockage of the pulmonary artery cuts off blood flow to the lung, disrupts oxygen exchange, and can lead to serious respiratory problems. Especially with large clots, sudden and severe conditions that can lead to cardiac arrest may develop.
What are the Symptoms of Pulmonary Embolism?
The symptoms of pulmonary embolism vary depending on the size of the clot, its location in the lung, and the patient’s general health condition. Small clots may only cause mild shortness of breath, while large clots can have fatal consequences.
Common symptoms include:
- Sudden onset of shortness of breath
- Chest pain (especially worsening with deep breathing)
- Cough, sometimes with bloody sputum
- Swelling and pain in the legs (especially if unilateral, may indicate DVT)
- Mild fever
- Cold sweats
- Rapid and irregular heartbeat
- Dizziness, feeling faint
- Rarely, loss of consciousness
Symptoms can be sudden and severe. Therefore, the presence of these symptoms in individuals with risk factors requires immediate medical attention.
What Causes Pulmonary Embolism?
Main Risk Factors:
- Prolonged immobility (bed rest, long journeys)
- Surgical operations (especially orthopedic and cancer surgeries)
- Pregnancy and postpartum period
- Hormone therapies and birth control pills
- Obesity
- Smoking
- Old age
- Clotting disorders (thrombophilia)
- History of deep vein thrombosis
The presence of one or more of these factors significantly increases a person’s risk of developing pulmonary embolism.
How is it Diagnosed?
To diagnose, the patient’s symptoms are first evaluated, followed by these tests:
- D-dimer test: Indicates increased blood clotting. However, it doesn’t provide a definitive diagnosis on its own.
- Lung CT angiography: The most reliable imaging method that definitively shows the presence and location of the clot.
- Ventilation-perfusion scintigraphy: Can be preferred as an alternative to CT.
- Doppler ultrasonography: Used to check for clots in the legs.
- ECG and chest X-ray: Performed to support diagnosis and for differential diagnosis.
What Happens if Pulmonary Embolism is Left Untreated?
If left untreated, approximately 30% of pulmonary embolism cases can be fatal. Complete blockage of the pulmonary artery by the clot can cause sudden cardiac arrest.
In the long term, untreated patients may develop chronic thromboembolic pulmonary hypertension (CTEPH). This condition means a permanent increase in pulmonary vascular pressure and can eventually result in right heart failure. This leads to persistent shortness of breath, weakness, and a significant decrease in quality of life.
What are the Treatment Methods?
Treatment is planned according to the severity of the embolism, the patient’s general condition, and underlying causes:
1. Anticoagulant (Blood Thinning) Treatment
This is the most commonly used method. It prevents the clot from growing and prevents new clot formation. Medications used include:
- Low molecular weight heparin
- Oral anticoagulants such as rivaroxaban, apixaban
- Warfarin (requires regular INR monitoring)
Treatment duration is usually 3-6 months. This period can be extended if the risk condition persists.
2. Thrombolytic Therapy (Clot-Busting)
Clot-dissolving drugs are administered intravenously in life-threatening or massive embolisms. Due to the risk of bleeding, it is only used in critical patients.
3. Surgical or Catheter-Based Clot Removal
In rare and advanced cases, the clot is directly removed or dissolved via catheter. These procedures require high technology and experience.
4. Oxygen Therapy and Supportive Care
Supportive treatment can be applied in mild embolisms. Oxygen support is provided if necessary, and bed rest is ensured.
How is Pulmonary Embolism Prevented?
The most effective way to prevent pulmonary embolism is to prevent the formation of deep vein thrombosis. The following measures are recommended especially for people in risk groups:
For patients confined to bed for long periods:
- Use of blood thinners
- Use of anti-embolism stockings
- Intermittent pneumatic compression devices
During long journeys:
- Walking at frequent intervals
- Drinking plenty of water
- Avoiding alcohol and smoking
In the post-operative period:
- Early mobilization
- Anticoagulant therapy
Pulmonary embolism is a serious vascular disease that can be life-threatening if not diagnosed early. Individuals with risk factors should be vigilant for symptoms and seek medical attention without delay. With appropriate treatment and preventive measures, it is possible to protect against this disease.
