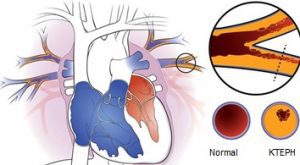
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is a life-threatening disease characterized by persistent blockage in the pulmonary blood vessels, often developing after a pulmonary embolism. When the blood vessels leading to the lungs narrow or become blocked due to clots, this can leave behind chronic thrombosis. Blood flow decreases in the blocked vessels, increasing vascular resistance within the lungs, leading to increased pressure known as pulmonary hypertension.
CTEPH does not only develop due to past embolism cases. In some cases, clot accumulation can occur in the pulmonary vessels without any history of embolism. It is more common in women than in men.
What Causes CTEPH? What Are the Risk Factors?
CTEPH development is associated with certain clinical conditions. These factors can both facilitate clot formation and cause chronic blockage in the pulmonary vessels.
Known Risk Factors for CTEPH:
- Previous pulmonary embolism
- Chronic inflammatory diseases (e.g., inflammatory bowel disease, osteomyelitis)
- History of cancer
- Individuals with a tendency to clot (thrombophilia)
- Prolonged bed rest
- Hormonal treatments and estrogen use
- Family history of clots
The presence of these factors can lead to the clot becoming permanent and cause irreversible damage to the pulmonary vascular system.
When and How Do Symptoms Appear?
CTEPH typically starts showing symptoms about 2-3 months after a pulmonary embolism. During this period, the patient may feel well; this phase is called the “honeymoon period” in medicine. However, symptoms then appear slowly and insidiously.
Most Common Symptoms:
- Shortness of breath: The earliest and most common symptom.
- Fatigue and exercise intolerance
- Chest fullness or pressure sensation
- Bluish discoloration of feet and hands (cyanosis)
- Signs of right heart failure in advanced stages
These symptoms progress slowly and can often be confused with asthma or COPD. Therefore, careful evaluation is necessary.
How is CTEPH Diagnosed?
Several different tests are used together to diagnose CTEPH. The main issue is that shortness of breath cannot be explained by other causes, and the disease is not considered.
Diagnostic Methods:
- Echocardiography (ECHO): Provides information about enlargement of the right side of the heart and increased pressure to the lungs.
- Ventilation/Perfusion Scintigraphy (V/Q Scan): The most sensitive imaging method for CTEPH. It shows the mismatch between lung ventilation and perfusion.
- Computed Tomography (CT) Angiography: Clearly shows the location of the clot and vessel blockages.
- Right Heart Catheterization: Directly measures lung pressure by entering the heart. It is critical for confirming the diagnosis and treatment planning.
How is CTEPH Treated?
The treatment approach varies depending on the stage of the disease, the pressure increase in the pulmonary vessels, and the extent of the clot. CTEPH can be successfully treated when diagnosed early.
1. Medical Treatment (Pressure Control with Medications)
- Used in patients with mild to moderate pulmonary hypertension.
- Pulmonary vasodilator drugs attempt to lower intrapulmonary pressure by dilating blood vessels.
- However, drug therapy is generally supportive and does not provide a permanent solution.
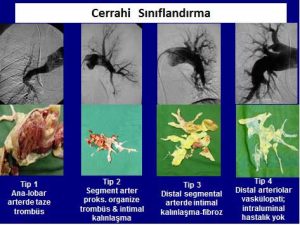
2. Surgical Treatment: Pulmonary Thromboendarterectomy (PTE)
- The most effective and definitive solution for CTEPH.
- Blocked vessels are cleared through open heart surgery.
- The surgery is performed under a heart-lung machine with deep hypothermia.
- This surgery, performed in experienced centers, significantly improves patients’ quality of life.
The earlier the surgery is performed, the higher the success rate. When lung pressure is very high or the right heart is severely affected, surgical risk increases.
3. Balloon Pulmonary Angioplasty (BPA)
- May be preferred for patients unsuitable for surgery or those who develop clots again.
- Narrow areas are widened with a balloon by accessing the pulmonary vessels with a catheter.
Can CTEPH be Prevented?
The most effective way to prevent CTEPH is timely recognition and proper treatment of pulmonary embolism. Therefore:
- Anticoagulant therapy should be regularly maintained in patients diagnosed with deep vein thrombosis.
- Patients who have had a pulmonary embolism should be closely monitored for symptoms during the honeymoon period.
- Prophylactic measures (blood thinners, compression stockings, early mobilization) should be applied for long-term bedridden patients.
Conclusion
Chronic thromboembolic pulmonary hypertension (CTEPH) is a serious condition that progresses insidiously but can be effectively treated if diagnosed in time. If individuals who have experienced pulmonary embolism have complaints such as shortness of breath, CTEPH should definitely be considered and necessary examinations should be performed. Early diagnosis and appropriate treatment play a critical role in increasing lifespan and quality of life.